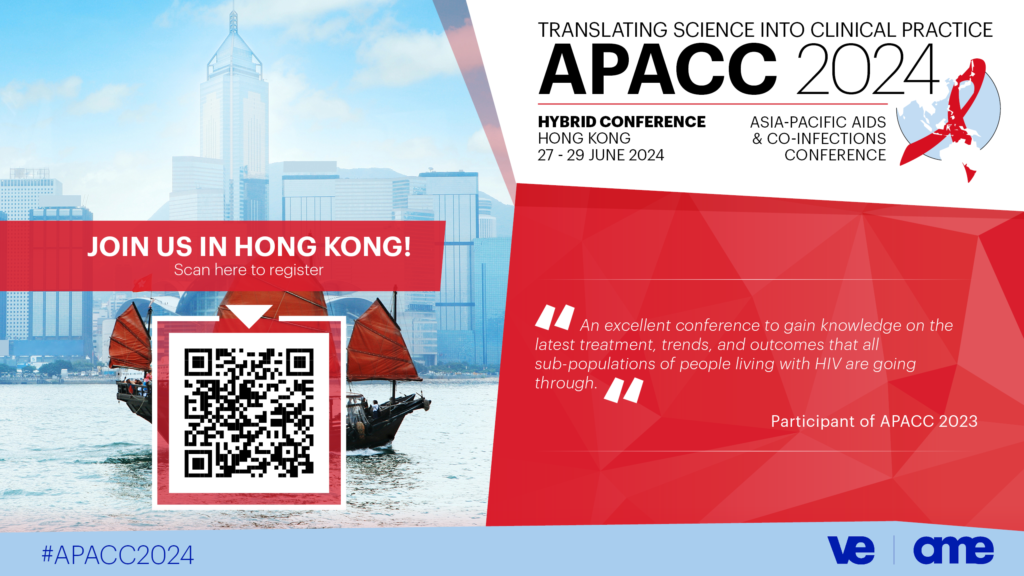
Join us at the Asia-Pacific AIDS & Co-Infections Conference (APACC) 2024! https://bit.ly/3HbmZmU
The Asia-Pacific AIDS & Co-Infections Conference provides a much-needed scientific platform that focuses on the developments, issues, and needs in the Asia-Pacific region.
Researchers have the opportunity to present and discuss the latest developments and are offered opportunities for interaction, networking, and building collaborations.
Top experts integrate science and clinical practice through state-of-the-art lectures, clinical case discussions, roundtable discussions, and debates in order to reach consensus on best practices and inform how treatment guidelines are implemented.
APACC 2024 will be held as a hybrid conference from 27-29 June 2024. We invite you to join us and we look forward to seeing you there!
Register Here: https://bit.ly/3HbmZmU
Learn more here: https://academicmedicaleducation.com/meeting/apacc-2024
and on LinkedIn and Facebook: @AcademicMedicalEducation, and X/Twitter: @Academic_MedEdu.
See you at #APACC2024! |